Over the past 15 years, there have been six Public Health Emergencies of International Concern (PHEIC) since the creation of the International Health Regulations in 2005. These PHEIC’s include the 2009 H1N1 Pandemic, Ebola (West African outbreak 2013-2015, outbreak in Democratic Republic of Congo 2018-2020), poliomyelitis (2014 to present), Zika (2016) and the current COVID-19 pandemic. These PHEICs have often been entangled with some of the world's worst humanitarian crises or occurring in areas with fragile health systems. Most of these complex crises, compounded with PHEICs, have been going on for years - if not decades - ranging from the Civil War in Syria, ongoing conflict in DRC and famine in Yemen to ongoing climate change events like droughts, food insecurity, and recurring disease outbreaks. These humanitarian crises are only further exacerbated by the COVID-19 pandemic, which is the latest PHEIC declaration by the World Health Organization.
Over the course of the history of the humanitarian aid sector, thousands of humanitarian aid workers, including public health, medical and crises response experts from the United States and other nations have been deployed for decades developing and sharpening the technical skills needed in health crises. These experiences and skills can provide a framework to help strengthen health systems, risk communication and community engagement strategies, vaccine rollouts, recovery and overall public health funding in the U.S.
During a seminar discussion, experts from the United Nations, World Health Organization and the World Bank joined to discuss vital lessons learned from shared recommendations for change. Below are 7 key recommendations that should be applied to the current global COVID-19 pandemic and be part of future health crises moving forward.
|
1. Boots-on-the-ground Community Engagement |
From preparedness to response to recovery begins and ends at the community level. Building trust within communities requires trusted messengers. There is no successful response without boots on the ground community engagement, which also includes ongoing feedback from the community. |
|
2. Incorporate Mental Health into Response
|
Mental health and Psychosocial Support (MHPSS) have been long overlooked. We must create a culture of safety and prioritize mental health just like physical safety into response, especially with protracted crises. |
|
3. Secondary effects from a global health crisis, such as from the COVID-19 pandemic should be acknowledgement and addressed as part of primary response
|
Secondary effects from a global health crisis (i.e., COVID-19 Pandemic) such as delays in routine immunizations and seeking health care services for non-COVID-19 related conditions should be incorporated into the preparedness plan and response, not addressed apart. |
|
4. Investment and Structuring of Human Resources and Human Capital
|
The biggest asset in any health crisis is human resources. There must be investment and strategic approach to workforce development, “tiered” recruitment and rosters, and additional investment in human capital. |
|
5. Investment in Health Systems and Public Health Strengthening
|
Investment in health systems and public health strengthening to allow for rapid detection of outbreaks and early warning systems (e.g. workforce, laboratories, robust surveillance systems, finance, Emergency Operations Centers) not only during emergencies and outbreaks but lulls as well. |
|
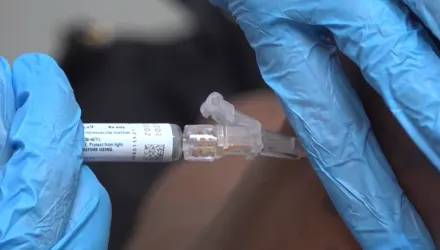
6. Improve Access to Routine Vaccines and Health Care Services
|
Improving access to health care services via community-based approaches, focus on primary care and investing in infrastructure such as vaccine manufacturing at the national level. |
|
7. Investment in Emergency Preparedness through Whole-of-Government Approaches
|
A pandemic requires an all-hands-on-deck emergency management approach involving all stakeholders and as such must be treated through a coordinated and collaborative fashion. Having emergency management plans for how to coordinate with clear roles and responsibilities remains paramount in addition to using command and control such as through an incident management structure. |
Madad, Syra, Sabs Quereshi, Dr. Linda Mobula, Dr. Ambrose Otau Talisuna and Dr. Esther Tan. “Applying Lessons from Other Global Crises to the COVID-19 Pandemic and Future Health Crises.” Belfer Center for Science and International Affairs, Harvard Kennedy School, January 12, 2022