As influenza activity increases this winter, many people are hearing unfamiliar labels like influenza A(H3N2) “subclade K” (J.2.4.1) and wondering whether they signal a more dangerous wave. The truth is that viral evolution is constant and new genetic branches can spread quickly without necessarily changing the clinical picture.
Here are 3 things the public should know about influenza A(H3N2) “subclade K” (J.2.4.1) and what we’re seeing in the U.S. right now.
- Subclade K is a genetic branch of H3N2, and evidence so far suggests it is not more severe
Influenza viruses constantly mutate through “drift.” Subclade K (J.2.4.1) is a newer genetic branch within influenza A(H3N2) that has risen quickly since August 2025 in multiple countries. The key point is reassuring: current epidemiologic data do not show increased disease severity from subclade K compared with other seasonal flu strains. This is more about viral evolution and spread than a “super flu.”
- The vaccine may be a less perfect match for subclade K, but it still matters most for preventing hospitalization
CDC reports these subclade K viruses are antigenically “drifted” compared with the H3N2 component selected for U.S. 2025 to 2026 vaccines, so protection against milder illness could be lower than in a well-matched year. But the outcome that matters most is severe disease. Early real-world data from England show vaccine effectiveness against flu related hospitalization in typical ranges, roughly 70 to 75% in children and 30 to 40% in adults, and even with drift, vaccination still helps prevent severe outcomes and can reduce spread. In addition, surveillance to date has not shown evidence that subclade K has reduced susceptibility to recommended antivirals, such as oseltamivir, zanamivir and baloxavir, so antivirals are still expected to be effective when used.
- In the U.S., subclade K is now dominant among genetically characterized H3N2 viruses, flu activity is rising, but severity indicators remain low (so far)
CDC’s latest FluView update for the week ending Dec. 13th reports influenza activity continues to increase across the country, with A(H3N2) the most frequently reported subtype. Among H3N2 viruses that CDC genetically characterized since late September, almost 90% were subclade K, making it a likely major driver of this winter’s H3N2 season. CDC also estimates that so far this season there have been at least 4.6 million illnesses, 49,000 hospitalizations, and 1,900 deaths, and three pediatric flu deaths have been reported to date, including two reported in the most recent week.
What people should do:
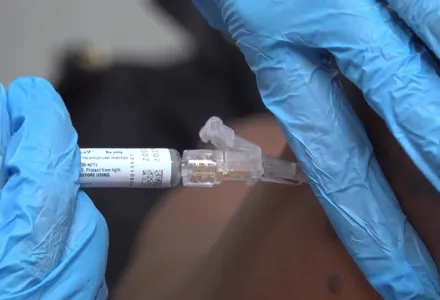
- Get vaccinated if you haven’t yet this season (especially if you’re 65+, pregnant, immunocompromised, or have chronic conditions).
- If you get sick and you’re high-risk (or caring for someone who is), ask quickly about antivirals, they work best when started early.
- Layer the basics: stay home when febrile/sick, and consider masking in crowded indoor spaces when respiratory viruses are surging locally
- Seek urgent or emergency care for warning signs such as difficulty breathing, persistent chest or abdominal pain, confusion or inability to wake, seizures, not urinating, severe weakness, or symptoms that improve and then return or worsen.